2nd International Pilonidal Conference Summary
Presentations
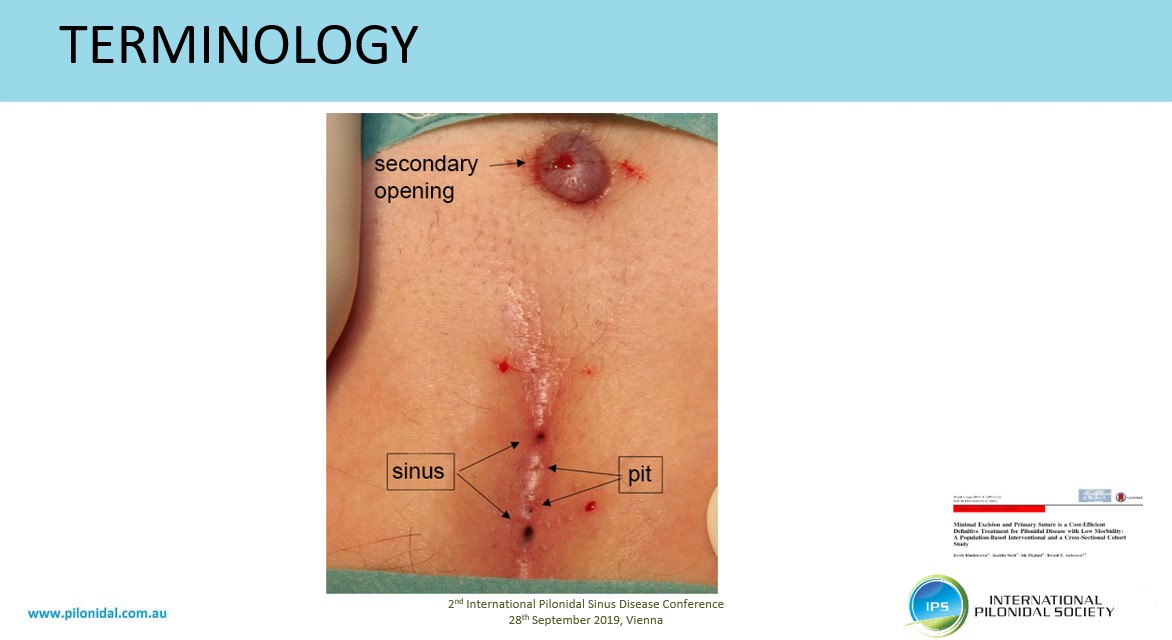
Peter Wysocki - General Surgeon, Logan Hospital and Sunnybank Private Hospital, Brisbane, Australia: Pilonidal Sinus morphology and terminologypowerpoint
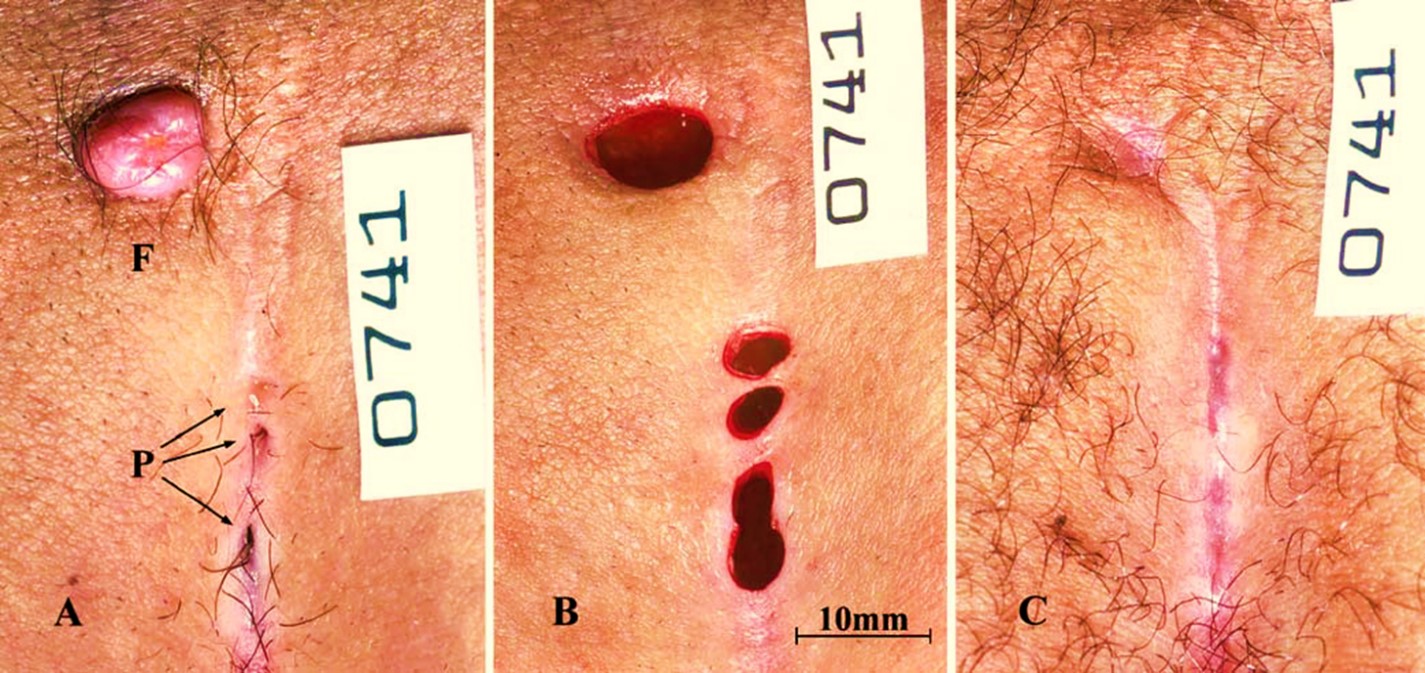
Macroscopically there may be midline tiny pits or (classically) larger sinuses. There may be a secondary opening which is typically superior and to left. Disease may be considered as primary, unhealed wound, recurrence or new primary. Differential diagnosis includes hidradenitis suppurativa. Hair has scales and due to friction hair migrates in leading with the root end. Source of hair in 14 pilonidal sinuses was predominantly from head (70%) but also from buttocks (60%) and lower back (60%). Simple classification may be: acute, mild or severe.
Prof. Dr. Dr. Dietrich Doll, St. Marienhospital Vechta: Times are changing – so what about PSD changing?
Incidence of pilonidal sinus in civilian and military populations is increasing. Peak onset is age 15 years. Recurrence rate depends on length of follow-up, type of procedure and country. Proposed establishing Centres of Pilonidal Sinus Surgery: 20 pts per year over three years, practice portfolio of methods, standardized reporting.
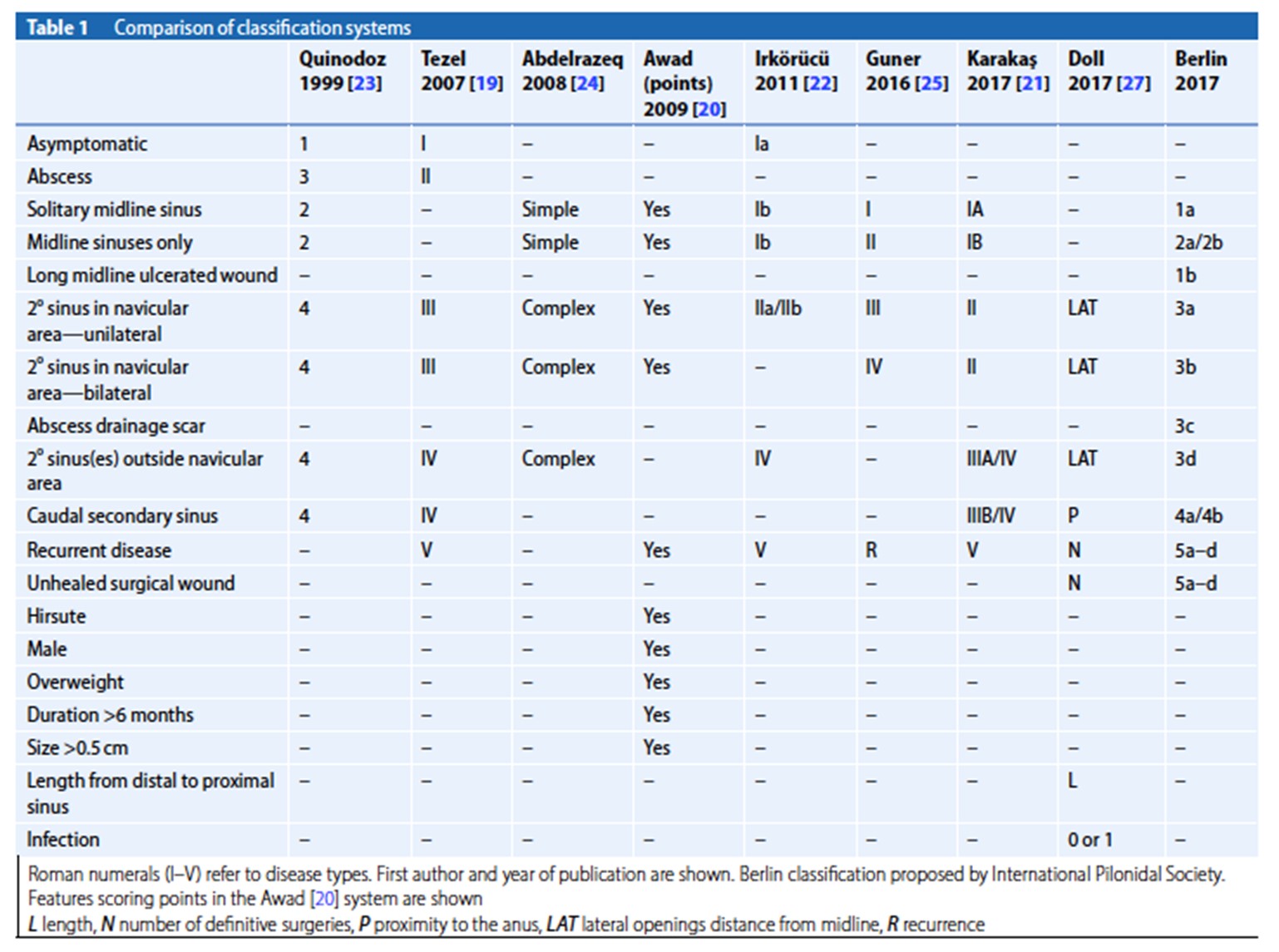
Ekmel TEZEL, MD, PhD - Gazi University, Ankara, Turkey: Pilonidal classıfıcatıon
Miss Rhiannon L Harries: Post CCT fellow in Abdominal Wall Reconstruction, Exeter: Challenging Wounds: Pilonidal Sinus
Welsh Wound Innovation Centre experience: Wound hygiene Shaving Silver nitrate to suppress overgranulation Lay open skin bridges Inadine roll and gauze roll Oral Antibiotics (usually Clarithromycin and Metronidazole) Topical steroid ointment for surrounding dermatitis Topical anti-fungal if fungal disease Prontosan® irrigation NPWT
Farida Benhadou, MD: Dermatology, Erasme Hospital, Brussels: Relationship between Hidradenitis suppurativa and Pilonidal sinus disease
One subtype of HS (phenotype LC2) is associated with pilonidal sinus. HS sinuses show hyperpigmentation but no hair within the sinus. Of 2100 patients, 26% described an intergluteal lesion and 80% of these were diagnosed as a pilonidal sinus (454 patients or 21% of cohort). Patients require multidisciplinary care as recurrent intergluteal fold lesions may be treated with systemic treatment (for HS).

Steven Immerman MD, FACS - Eau Claire, Wisconsin, USA: The Long Distance Patient
Clinical assessment, potential for revision surgery discussed, day case operation, email follow up. Typically no post-operative visits.

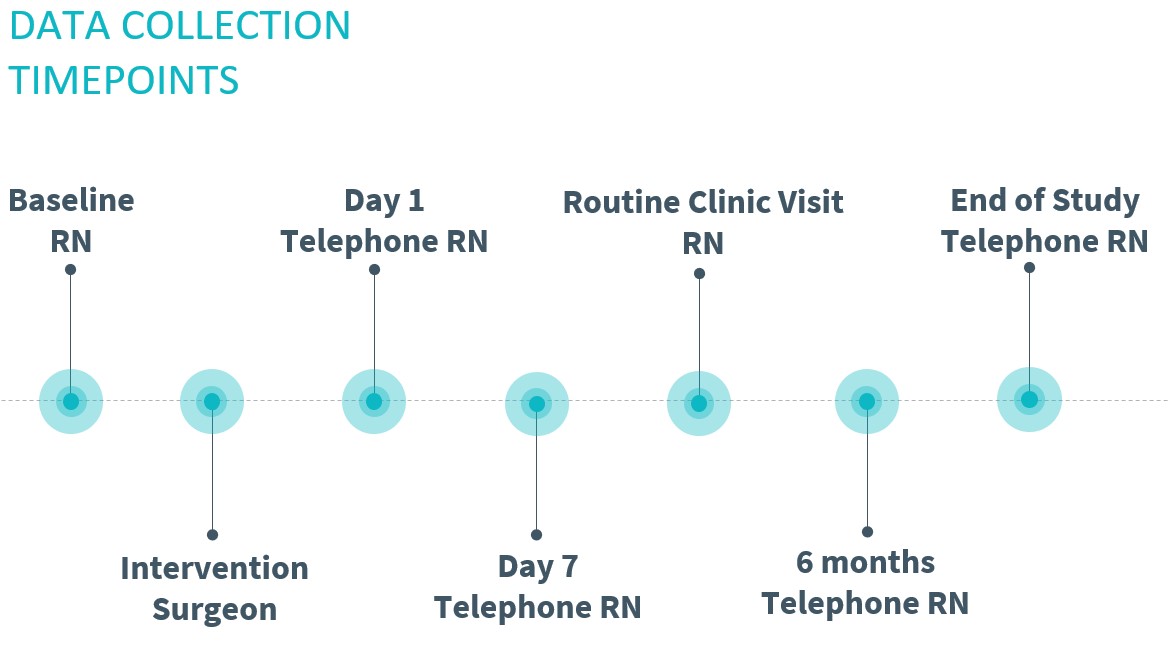
Professor Steven Brown: The University of Sheffield: The PITSTOPStudy: PIlonidal sinus Treatment: STudying the Options
Observational cohort with mixed methods qualitative elements which aims to: Inform subsequent comparative trials Validate a Classification Describe front running treatments and how they are done Patient relevant outcomes

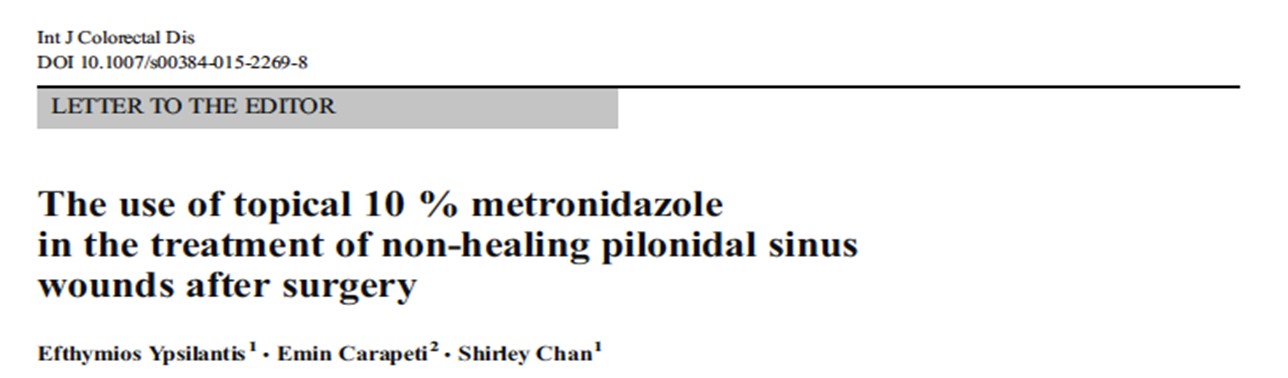
Emin Carapeti BSc MB BS MD FRCS, Consultant Colorectal Surgeon, London: Role of ORTEM for Non-Healing sacrococcygeal wounds
ORTEM SLA Pharma (10% metronidazole) should be tried as first line treatment. It has a high success, is low cost and safe.
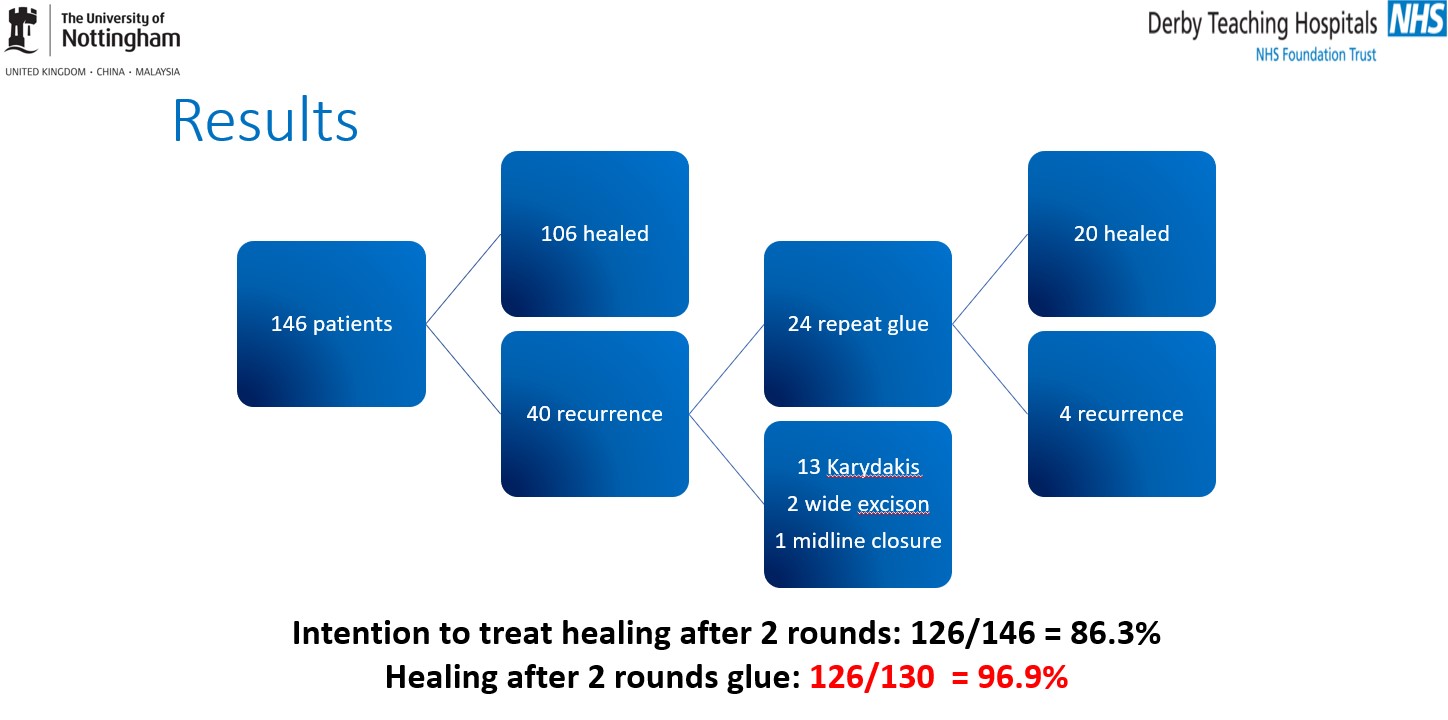
Tanvir Singh Sian, Jon Lund - Department of Colorectal Surgery, Royal Derby Hospital, UK: Fibrin Glue in the treatment of Pilonidal Sinus Disease
Published in Techniques Coloproctology 2018, 22(10): 779-84. Quick and cheap procedure. High patient satisfaction. No aftercare / dressing requirements. Early return to normal activity.
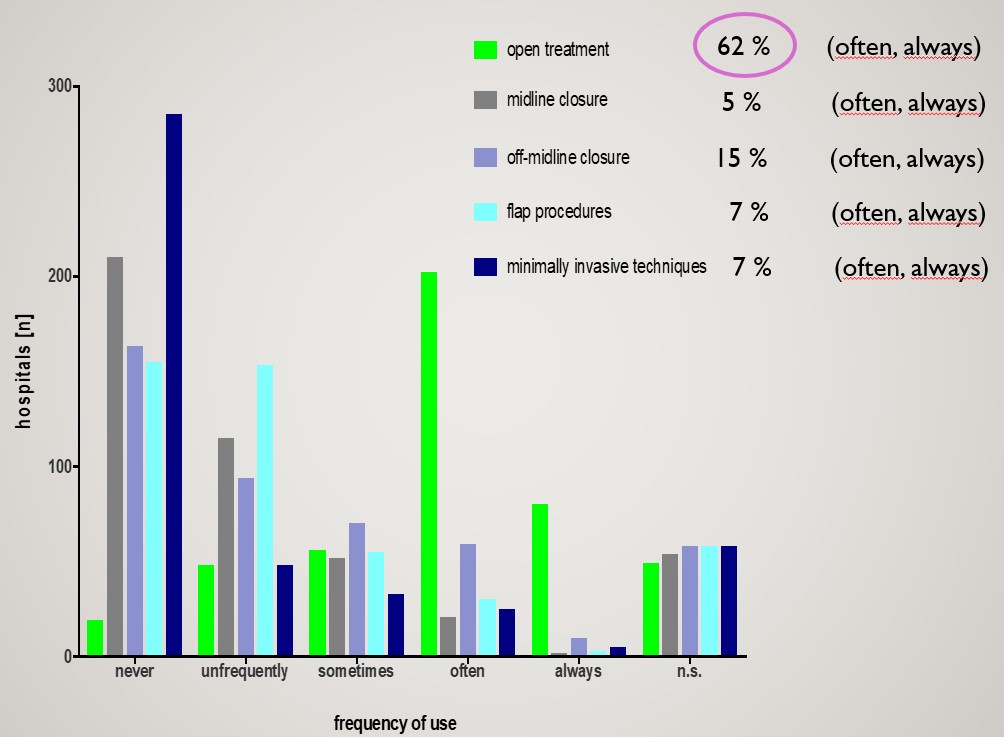
Prof. Dr. Dr. Dietrich Doll, Nora Peters: The spectrum of surgical PSD therapy in Germany
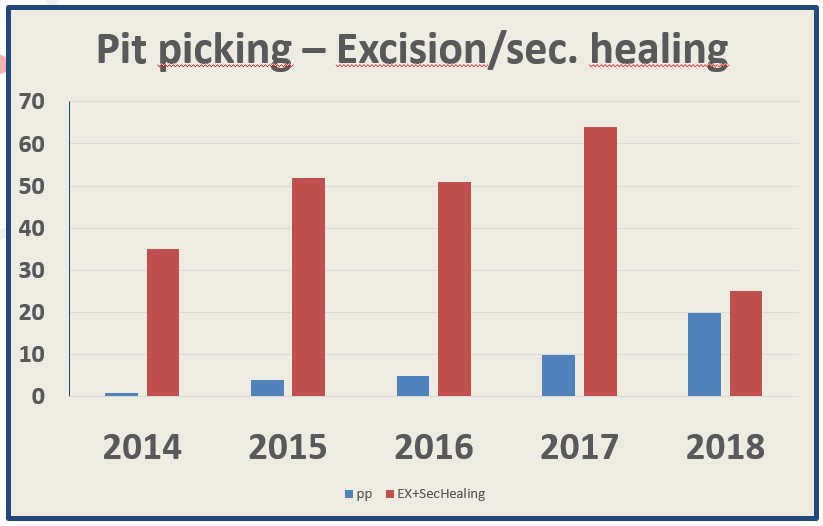
Johannes Jongen - Kiel, Germany: What I / We learnt from doing Pit Picking
Preop: NO bowel prep Surgery: Local anaesthesia, outpatient setting Shaving of the surgical site NO Antibiotics Excision of the pits with a trephine (4 mm) Rinsing the wound with saline Postoperative: Showering the wound Gauze with ointment (dexpanthenole) Analgetics ad lib
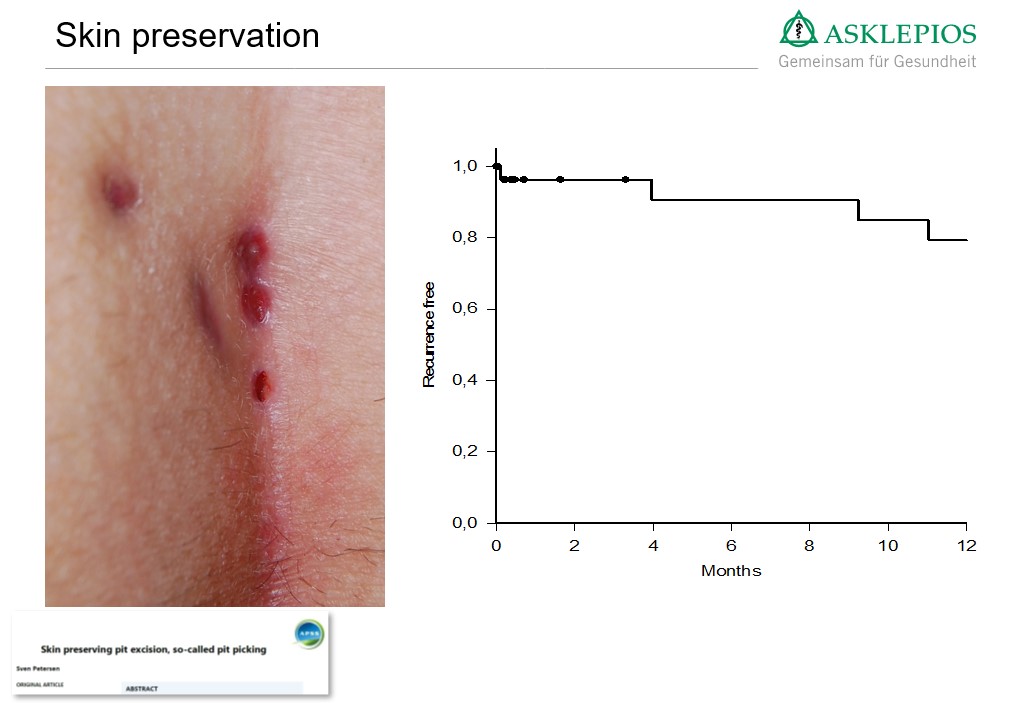
Sven Petersen - Asklepios Klink Altona, Abteilung für Allgemein- Viszeral- und Gefäßchirurgie: Skin Preserving Pit Excision
Dr. M. Gips (presented with permission by P Wysocki): Minimal Surgery for Pilonidal Disease Using Punches (Trephines)
powerpoint
The pilonidal units (midline and secondary openings) can be treated individually, without compromising the surrounding uninvolved tissues, even if some units are interconnected subcutaneously. Pit excision thus preserves healthy skin and fat. Recurrence rate 16% at 10 years.
Roland E Andersson - Linköping University, Linköping, Sweden Modified Lord Millar: What your patient needs to know
Prof. Dr. Cuneyt Kayaalp - Department of Gastrointestinal Surgery, Inonu University, Malatya, Turkey: Role of Phenol
Among the minimally invasive treatments, phenol is the most researched, experienced method. May reduce the morbidity when compared with pit excision alone but impact on recurrence is not clear.
Prof. Marco Milone, MD, PhD - University of Naples «Federico II»: Video of EPSiT / VAAPS presented
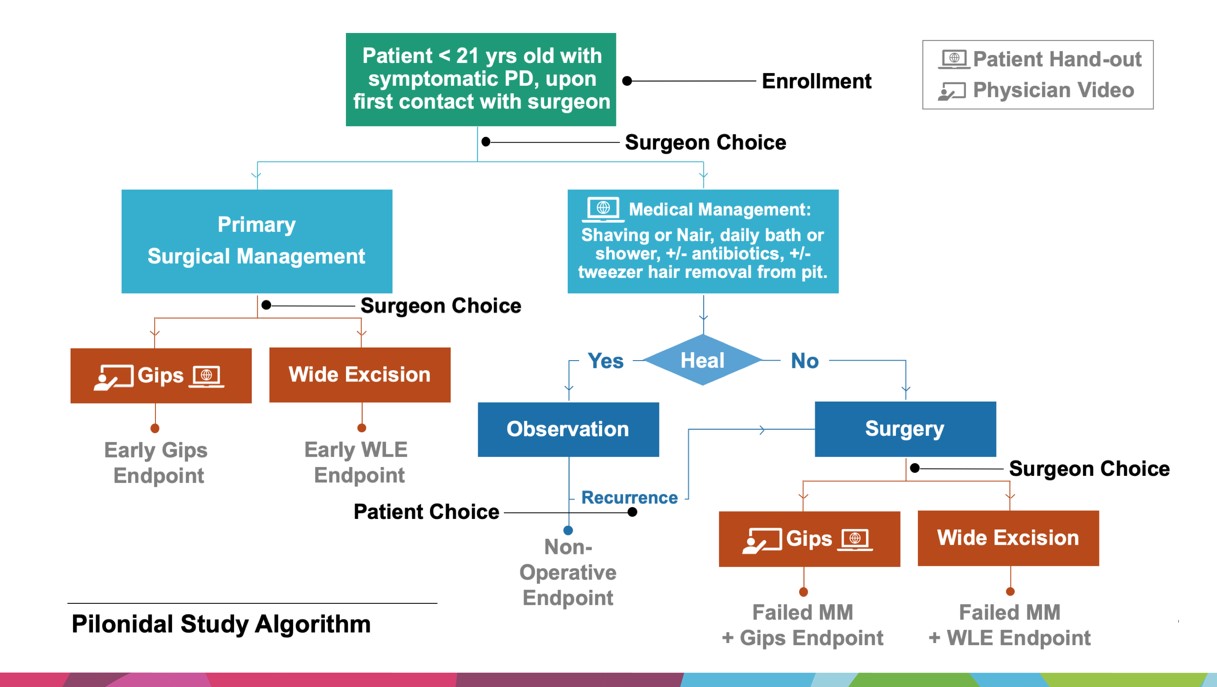
Nelson G. Rosen MD – Cincinnati Children’s: Pilonidal Disease – The Midwest Pediatric Surgery Consortium Project
powerpoint
Asha Senapati - St Mark's Hospital, London, UK: Bascom cleft lift
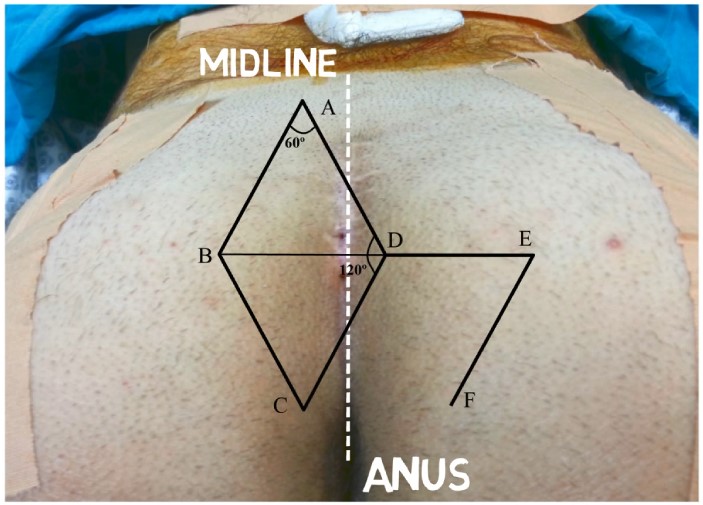
Mehmet Kaplan - Associate Professor, NCR International Hospital, Gaziantep: Limberg Flap Design
One of the recommended flap designs is shown below (Kaplan Type 6). This is the least performed and probably the best. Points “A” and “C” are 2cm from midline
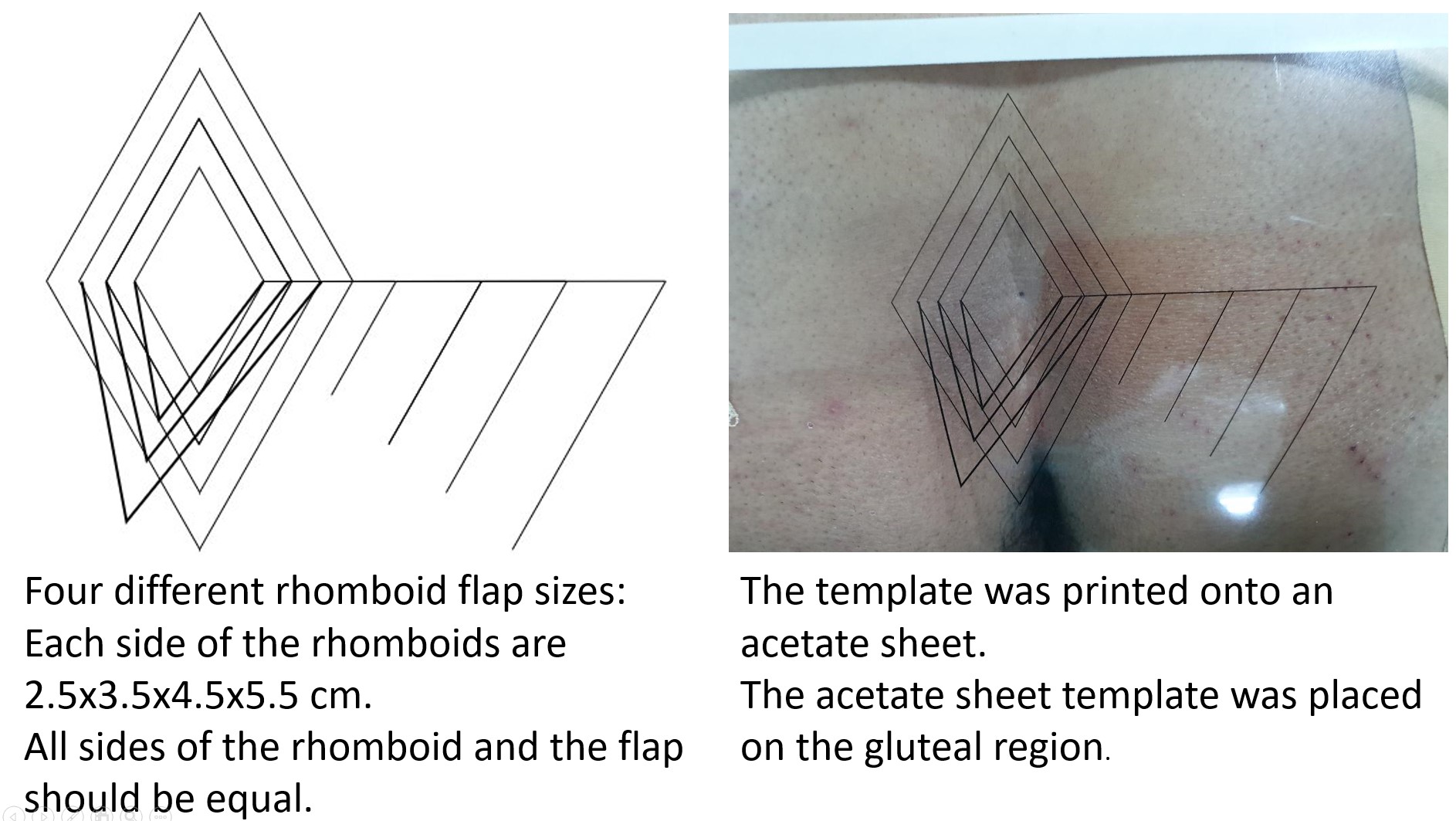
Dr. Mehmet Eren Yüksel - Ankara Yıldırım Beyazıt University, School of Medicine, Intensive Care Unit, Ankara, Turkey: Standardization Of Modified Limberg Flap Technique By Using An Acetate Template For The Management of Pilonidal Disease
powerpoint
Using a standardized template while performing modified Limberg flap surgery may help to evaluate the outcomes of this technique more accurately.
Peter Wysocki - General Surgeon, Logan Hospital and Sunnybank Private Hospital, Brisbane, Australia: Karydakis flap
powerpoint
Recurrence at 10 years 3% (DOI:10.1038/s41598-018-20143-4). Learning curve 10 – 20 patients depending on volume. Pitfalls include: excising too much fat laterally, displacing caudal apex medially to spare lateral buttock skin and leaving dead-space, placing a drain.
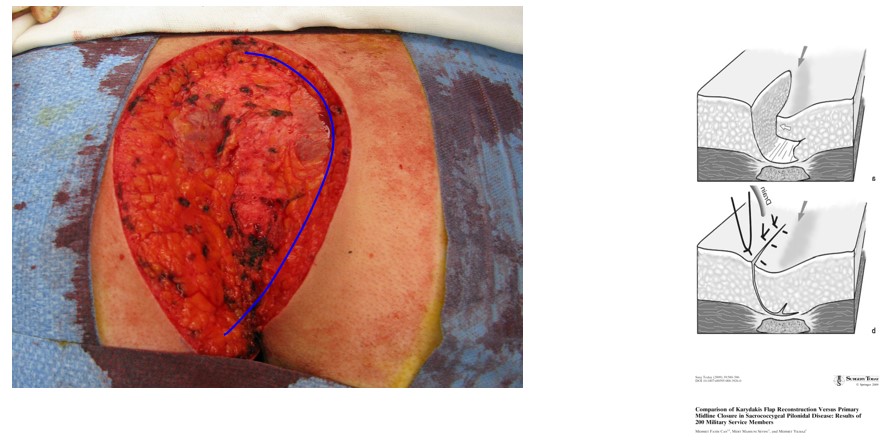
Igors Iesalnieks: München Klinik Bogenhausen, Munich, Germany: Managing the failed flap
The reason for failure is often a failure to lateralize the wound completely. Proposed that some type of recurrence prophylaxis is badly needed in patients treated for recurrent disease or failure of previous surgeries. One way of dealing with a distal failure after Karydakis flap is shown.

Steven Immerman MD, FACS - Eau Claire, Wisconsin, USA: Cleft Lift as a rescue
Tools and materials used in surgery: Scalpel, Electrocautery, Needle holders and Sutures, Blake drain, Steri-Strips, gauze, and tape, Experienced surgeon Video presented
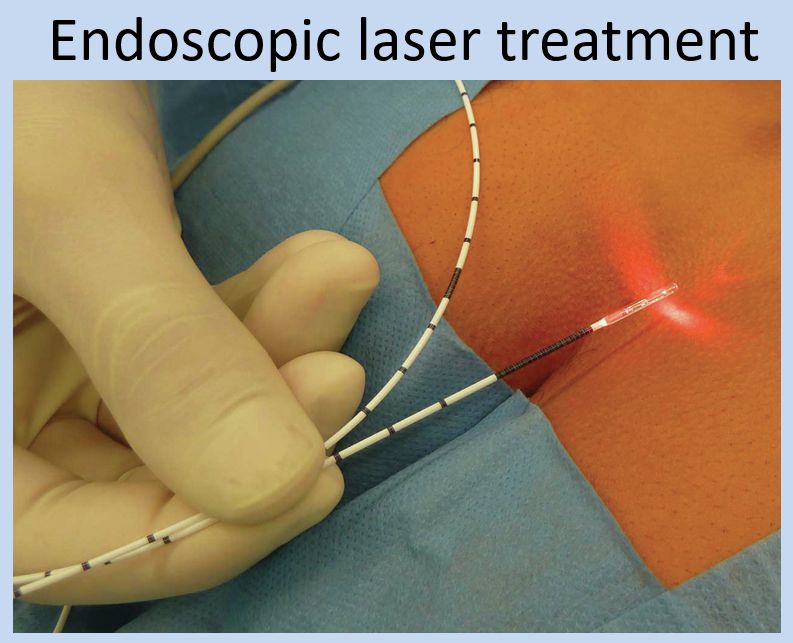
Georgios K. Georgiou – MD · MSc · PhD - General Surgeon, Metropolitan Hospital, Athens, Greece: OUTPATIENT TREATMENT OF PILONIDAL DISEASE USING A 1.470 nm DIODE LASER Video presented
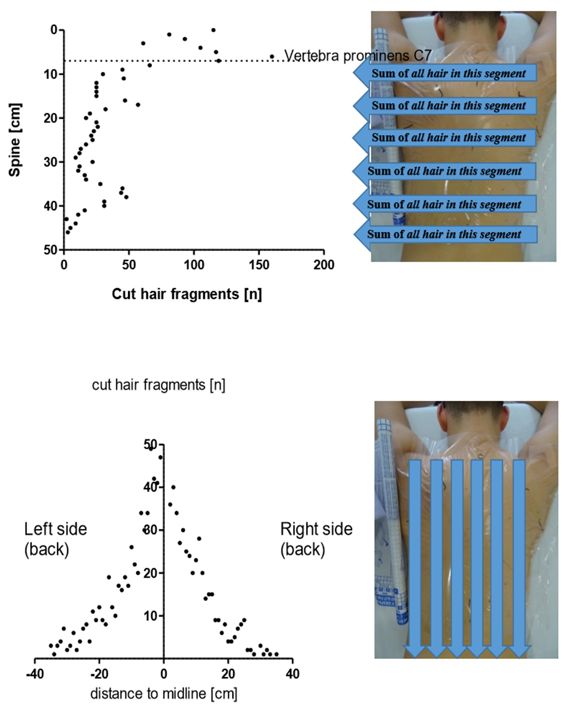
Prof. Dr. Dr. Dietrich Doll, St. Marienhospital Vechta: PSD, Hair and Haircuts
Data was shown in Berlin that axial strength of hair in patients with PSD is greater than controls (intergluteal hair 1.5g vs 0.7g p<0.0001). 8 male patients underwent a dry haircut using regular protective measures. This was followed by immediate cautious undressing and a 45x45 cm adhesive transparent sheet was placed on the dorsum. Cut hair and position were counted.
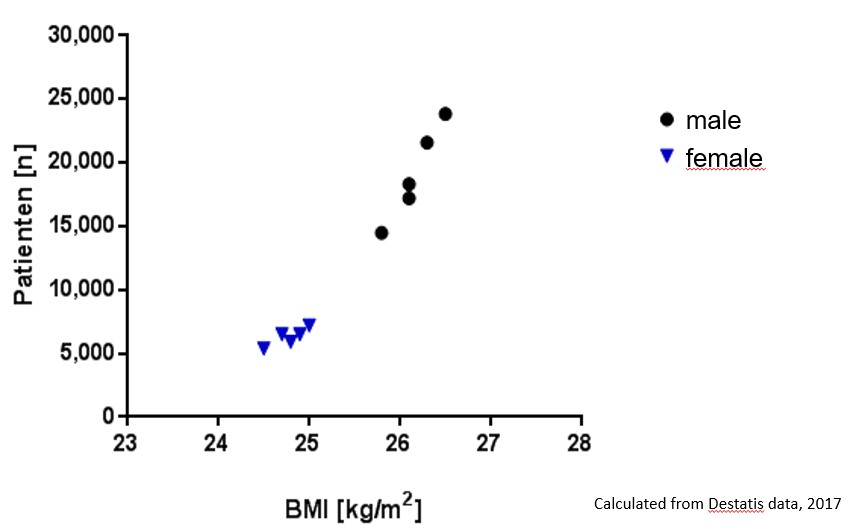
Prof. Dr. Dr. Dietrich Doll, St. Marienhospital Vechta: Influence of Body Mass Index on Pilonidal Sinus outcomes
In 2000’s incidence of pilonidal operations in Germany has increased more rapidly in men. Recurrence rate following midline closure or primary open treatment was 20% in obese and non-obese German soldiers (p = 0.9).
Peter Wysocki - General Surgeon, Logan Hospital and Sunnybank Private Hospital, Brisbane, Australia: Pilonidal abscess
Off-midline drainage is associated with quicker recovery than midline. Recurrence after pilonidal abscess drainage is 40% at 5 years. Perhaps not everyone requires definitive surgery after their first abscess drainage. About 1/3 of abscesses show no growth and more than 50% grow anaerobes.

